The prospect of moving procedures from the Operating Room to an ambulatory clinic setting can seem daunting.3 Patients are becoming more discriminating healthcare consumers and expect less invasive options in a more timely fashion that we have delivered in the past. Patients are asking to take an active role in their care, especially in situations where they can exert some control over scheduling, treatment, or procedures in a way that minimizes the impact on their life. In addition, the pandemic has challenged us to find new and innovative ways to deliver patient care.
One of the most common questions asked about enhancing the role of an ambulatory gynecology clinic is “where do I start”. A deliberate, step-wise consideration of the factors involved in this transition can make the process less intimidating and help us to better serve patients in an increasingly value-based care system. This article outlines steps you can take to keep your practice operating smoothly as you integrate ambulatory procedures.
Considerations for integrating procedures into the practice workflow4
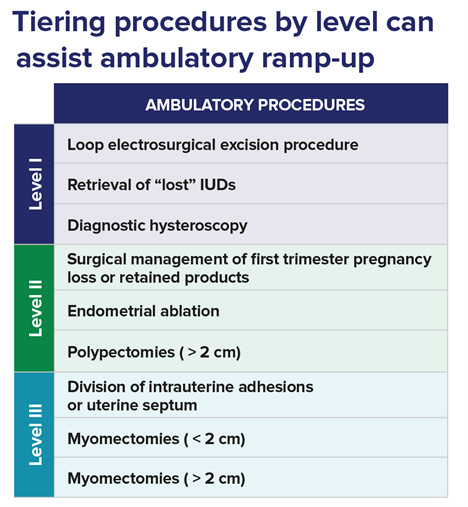
Choose the right ambulatory procedures. Carefully review everyone’s patient panel to identify the most common outpatient procedures. Recent surveys indicate that OBGYNs treat an average of 55 patients with abnormal bleeding per month.5 There are several procedures to treat abnormal uterine bleeding that can be performed in the ambulatory setting. In my experience, for example, most gynecologists are either performing or are interested in offering ambulatory endometrial ablations.5 You need not transition from the OR to an ambulatory setting that offers the full range of outpatient procedures all at once. Even if you are comfortable with all types of procedures in the OR setting, your nursing staff may not be, so a tiered introduction may lead to greater acceptance and successful adoption. You may choose to implement this practice change gradually. Consider starting with diagnostic hysteroscopy, simple operative procedures like polypectomy, then ablation, and finally more advanced procedures like adhesiolysis, septoplasty, and myomectomy. For optimal efficiency, it makes sense to limit the expansion of ambulatory to common procedures while avoiding those that are complex and rarely performed. This limits the possibility of disruption and stress caused when staff are asked to participate in unfamiliar procedures.6
Staff capacity and capabilities. Consult with your nursing and support staff to ensure they have the interest, skill, capacity, and training to support ambulatory procedures.7 Engage one or two champions to ensure you have staff buy-in and support for the integration. Work with a “point person,” to familiarize staff with the management of the procedure room and procedural protocols and to help with logistical oversight of ambulatory procedures.6 Consider the skill sets of each member of the current staff and the role each team member will play in procedural support. Ensure that any new responsibilities are within the team member’s scope of practice and help to provide the development and presentation of the necessary in service sessions.6For most procedures a nurse qualified to provide intravenous sedation or an anesthesiologist may be required. The staff assisting with circulation, pre and post-operative care as well as housekeeping and those tasked with care and maintenance of the equipment may also require additional in service.
Clinic layout and exam room space. You don’t need to replicate the surgical theatre to perform ambulatory procedures. In fact, you should consider doing just the opposite. Instead of a sterile, unwelcoming environment, create a comfortable and safe space for patients with artwork and music in your procedure room. A basic planning rule is that the space should easily accommodate all members of your support staff during the procedure. In addition, space will be needed in or near the procedure room for patient preparation and recovery.6 Most patients can recover in reclining chairs although it is useful to also have access to stretcher beds on occasion.
Proper equipment and supplies. The necessary diagnostic and surgical equipment will depend on the procedure(s) being performed. Adequate lighting is essential. Therefore, in addition to procedure-specific instruments and equipment, lighting upgrades may be necessary.6 Your clinic should determine if an automated exam bed and ergonomically designed and/or space-saving equipment profiles would make movement in the room easier or procedures more efficient.6 Consider the example of ambulatory-based hysteroscopy. When offering this outpatient service, six basic types of equipment are needed:9
- Diagnostic or operative hysteroscope
- Light source
- Camera
- Monitor
- System for uterine distention and fluid management
Once you have identified which procedures you plan to incorporate in your ambulatory center, perform an internal audit of your equipment to ensure you have all the instruments needed to be successful.
Scheduling. Among the many benefits of working in an ambulatory clinic is the ability to deliver less invasive procedures to a larger number of patients in the same amount of time with less risk and similar or better outcomes. Patients are able to walk in and out of the procedure room, turnover times are significantly reduced and patients spend less time in hospital thus reducing nursing cost as well as reducing exposure to pathogens. As opposed to the Operating Room where the minimum booking time for most centers is 60 minutes for even the simplest of procedures, once comfortable a clinic can schedule an hysteroscopy in the same room every 30 minutes.9 Companies such as Hologic can put you in touch with other practices and clinicians that have arranged their schedule in an efficient way that works well for the clinicians, staff, and patients.
Summary
While it may seem like a considerable effort, your current ambulatory center may have already applied many of these planning and execution steps which makes it amenable to the addition of gynecologic ambulatory procedures. A phased approach to integration can help you and your colleagues from feeling overwhelmed or like you have taken on an insurmountable task. Phased approaches also help stagger the costs so you can start to see early returns from simple procedures as you and your staff become more comfortable with complex procedures. Patients also benefit and are often the best advocates with their friends and family physicians. Preparing now to integrate ambulatory procedures into existing workflows can position a clinic to provide better access with for improved patient outcomes and satisfaction.
Dr. Thiel is a paid consultant of Hologic. Hologic provided editorial support for this article.
1..Wieand E, Lagrew Jr, DC. Value-based payment: what does it mean, and how can ObGyns get out ahead? OBG Management. 2018;30(1):17-26. 2.Witt M. In-office hysteroscopy procedures: reimbursement jumps 237%. OBG Management. 2017;29(7):26-29. 3. Cholkeri-Singh A. The benefits of integrating in-office hysteroscopy. MDedge web site. Accessed February 19, 2019. 4. Data on file. Hologic, Inc. 2018. 5. Data on file. Hologic, Inc. 2015. 6. Emery JD, Paraiso MFR, eds. Office-Based Gynecologic Surgical Procedures. New York, NY: Springer Science+Business Media; 2015. 7. Data on file. Hologic, Inc. 2016. 8. Cholkeri-Singh A. Payment changes drive hysteroscopy to the office. MDedge web site. Accessed February 19, 2019. 9. Wong M, Miller V. Why you should be performing office hysteroscopy...now. Contemporary OBGYN web site. Accessed February 19, 2019. 10. The American College of Obstetricians and Gynecologists. Report of the Presidential Task Force on Patient Safety in the Office Setting. Washington, DC: The American College of Obstetricians and Gynecologists; 2010.
 Dr. Thiel is a Clinical Professor and the Unified Head of Obstetrics and Gynecology at the University of Saskatchewan. He received his BSc (1983), MSc (1986) and MD (1991) from the University of Saskatchewan and received his Royal College Fellowship in Obstetrics and Gynaecology in 1996. He is the Director of the Postgraduate Fellowship Program in Minimally Invasive Gynecology for the University of Saskatchewan. He has been awarded both the CREOG and APGO Excellence in Teaching Awards for resident teaching and the 2010 Golden Hysteroscope award for best hysteroscopy paper at the 39th Global Congress of Minimally Invasive Surgery. His clinical and research interests include intra-operative evaluation, hysteroscopic tubal sterilization, alternatives for fibroid management, endometrial ablation, and chronic pelvic pain. Dr. Thiel is the President of the Canadian Society for the Advancement of Gynecologic Excellence (CanSAGE).
Dr. Thiel is a Clinical Professor and the Unified Head of Obstetrics and Gynecology at the University of Saskatchewan. He received his BSc (1983), MSc (1986) and MD (1991) from the University of Saskatchewan and received his Royal College Fellowship in Obstetrics and Gynaecology in 1996. He is the Director of the Postgraduate Fellowship Program in Minimally Invasive Gynecology for the University of Saskatchewan. He has been awarded both the CREOG and APGO Excellence in Teaching Awards for resident teaching and the 2010 Golden Hysteroscope award for best hysteroscopy paper at the 39th Global Congress of Minimally Invasive Surgery. His clinical and research interests include intra-operative evaluation, hysteroscopic tubal sterilization, alternatives for fibroid management, endometrial ablation, and chronic pelvic pain. Dr. Thiel is the President of the Canadian Society for the Advancement of Gynecologic Excellence (CanSAGE).